Understanding Syncope: The Prevalence and Significance of Fainting
Related Articles: Understanding Syncope: The Prevalence and Significance of Fainting
Introduction
With great pleasure, we will explore the intriguing topic related to Understanding Syncope: The Prevalence and Significance of Fainting. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Understanding Syncope: The Prevalence and Significance of Fainting
Syncope, more commonly known as fainting, is a transient loss of consciousness caused by a temporary reduction in blood flow to the brain. This common phenomenon affects individuals of all ages, though its prevalence and contributing factors can vary significantly. Understanding the frequency, causes, and potential risks associated with syncope is crucial for promoting awareness, seeking timely medical attention, and potentially preventing future episodes.
Prevalence and Demographics
Fainting is a remarkably common occurrence, with estimates suggesting that approximately 15-35% of individuals will experience at least one episode in their lifetime. While syncope can affect anyone, certain demographics are particularly susceptible:
- Age: The incidence of fainting increases with age, particularly in individuals over 65 years old. This is likely due to age-related changes in cardiovascular function and increased susceptibility to underlying medical conditions.
- Gender: While both men and women experience fainting, studies suggest that women may be slightly more prone to syncope, particularly during menstruation or pregnancy.
- Medical History: Individuals with pre-existing conditions like heart disease, low blood pressure, or neurological disorders are at an elevated risk of fainting.
- Medications: Certain medications, particularly those affecting blood pressure or heart rhythm, can increase the likelihood of syncope.
Causes of Syncope
Fainting can be triggered by a multitude of factors, broadly categorized into three main types:
- Neurocardiogenic Syncope (Vasovagal Syncope): This is the most common type of fainting, accounting for approximately 50% of cases. It is triggered by a sudden drop in blood pressure and heart rate, often in response to emotional distress, pain, or prolonged standing.
- Situational Syncope: This category encompasses fainting episodes related to specific situations, such as coughing, defecation, or urination. These instances are often associated with increased pressure in the chest or abdomen, leading to a temporary decrease in blood flow to the brain.
- Cardiac Syncope: This type of fainting is caused by underlying heart conditions, such as arrhythmias, heart valve problems, or coronary artery disease. It is often characterized by sudden and severe symptoms and requires immediate medical attention.
Diagnosing and Managing Syncope
Diagnosing the cause of fainting often involves a comprehensive medical evaluation, including:
- Medical History: A detailed account of the fainting episode, including the circumstances surrounding it, associated symptoms, and any pre-existing medical conditions.
- Physical Examination: Assessing vital signs, listening to the heart and lungs, and checking for any neurological abnormalities.
- Electrocardiogram (ECG): This test records the electrical activity of the heart, helping to identify potential heart rhythm irregularities.
- Echocardiogram: This ultrasound examination of the heart assesses its structure and function.
- Tilt Table Test: This test involves gradually tilting the patient’s body to simulate standing, helping to identify the cause of fainting associated with postural changes.
The management of syncope depends on its underlying cause. For neurocardiogenic syncope, strategies often include:
- Lifestyle Modifications: Avoiding triggers, such as prolonged standing, dehydration, and emotional stress.
- Medications: Beta-blockers and other medications may be prescribed to regulate heart rate and blood pressure.
- Cognitive Behavioral Therapy: This therapy can help individuals learn coping mechanisms for stress and anxiety, which can trigger fainting episodes.
For cardiac syncope, the treatment focuses on addressing the underlying heart condition, which may involve medications, surgery, or other interventions.
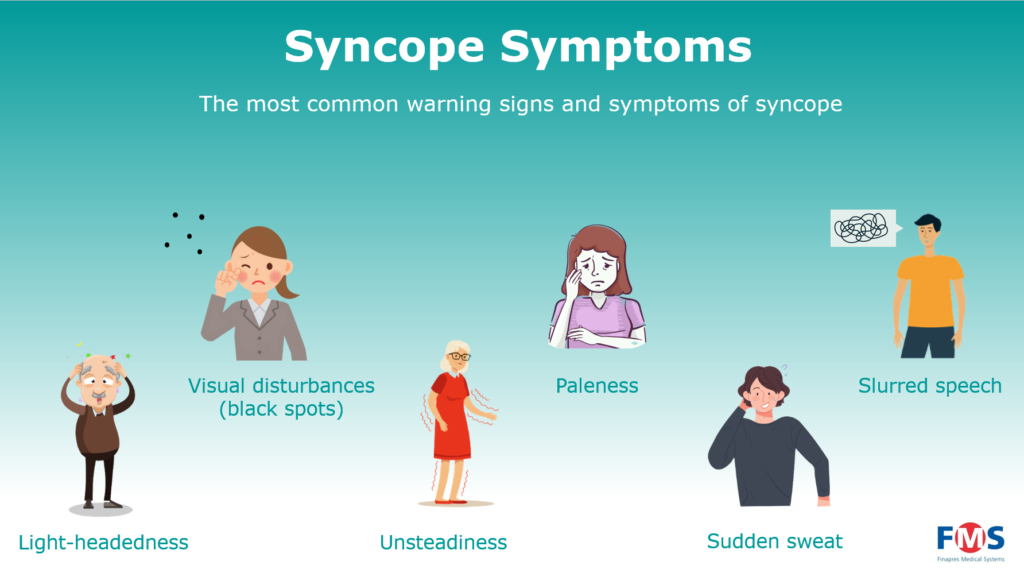
The Importance of Recognizing Syncope
While fainting is often a benign event, it can be a sign of a more serious underlying condition, particularly if it occurs frequently, is accompanied by other symptoms, or occurs in individuals with a history of heart disease. Recognizing the signs and symptoms of fainting is essential for seeking timely medical attention and receiving appropriate treatment.
FAQs
Q: How can I prevent fainting?
A: Preventing fainting often involves addressing the underlying cause. This may include:
- Hydration: Staying well-hydrated helps maintain blood volume and blood pressure.
- Avoidance of Triggers: Identifying and avoiding situations that trigger fainting, such as prolonged standing, emotional stress, or certain medications.
- Regular Exercise: Maintaining physical fitness can improve cardiovascular function and reduce the risk of fainting.
- Medical Management: Consulting a healthcare professional to address any underlying medical conditions or to explore medication options.
Q: When should I seek medical attention for fainting?
A: It is advisable to consult a doctor for any fainting episode, especially if it:
- Occurs frequently.
- Is accompanied by chest pain, shortness of breath, or other unusual symptoms.
- Is the first episode in an individual with no prior history of fainting.
- Is experienced by an individual with a history of heart disease or other medical conditions.
- Leads to injury or loss of consciousness for an extended period.
Q: What are the potential risks associated with fainting?
A: While most fainting episodes are harmless, potential risks include:
- Injury: Fainting can lead to falls and other injuries, particularly in older individuals or those with underlying medical conditions.
- Complications from Underlying Conditions: Fainting can be a symptom of a more serious underlying condition, such as heart disease or a neurological disorder, requiring prompt medical attention.
- Recurrence: Fainting can recur, particularly if the underlying cause is not addressed.
Tips
- Stay Hydrated: Drink plenty of fluids throughout the day, especially during hot weather or when engaging in physical activity.
- Avoid Triggers: Be aware of situations that trigger fainting and take steps to avoid them, such as standing for long periods, dehydration, or emotional stress.
- Regular Checkups: Schedule regular checkups with a healthcare professional, especially if you have a history of fainting or underlying medical conditions.
- Carry Emergency Information: Keep a medical identification bracelet or card with information about any medical conditions, medications, and allergies.
- Seek Prompt Medical Attention: Do not hesitate to consult a doctor for any fainting episode, particularly if it is accompanied by other symptoms or if you have a history of heart disease.
Conclusion
Fainting is a common phenomenon that can be caused by a variety of factors. While most episodes are harmless, it is essential to be aware of the potential risks and seek medical attention if necessary. Understanding the causes, triggers, and potential complications of fainting empowers individuals to take proactive steps to minimize their risk and ensure timely medical intervention when required. By promoting awareness and encouraging prompt medical evaluation, we can contribute to the well-being of those affected by this prevalent medical condition.








Closure
Thus, we hope this article has provided valuable insights into Understanding Syncope: The Prevalence and Significance of Fainting. We appreciate your attention to our article. See you in our next article!
